10 Things You Need To Know About Living with Genital Herpes

Living with genital herpes is often depicted — incorrectly — as a rare and embarrassing experience that’s unmanageable and untreatable.
But the truth is, genital herpes is relatively common in the United States. About one in every six people ages 14 to 49 in the U.S. is living with genital herpes right now, and all of them have the means to keep their condition under control. Thanks to antiviral medications and other breakthrough treatments, genital herpes doesn’t have to define you or your relationships!
If you’re living with genital herpes, keep scrolling. We’ll share 10 useful tips to help you live a full and satisfying life!
1. Research STIs
If you’re a sexually active person, understanding the symptoms of sexually transmitted infections, or STIs, is a crucial part of maintaining your overall health and well-being.
Below are some of the most common STIs and their primary symptoms:
- The herpes simplex virus (HSV), or genital herpes, can cause outbreaks of blisters on the genitals, rectum, upper thighs, or mouth. These painful sores can make living with genital herpes a challenge, but with proper care and knowledge, you can fight back and live a normal life.
- Chlamydia is a bacterial infection that can cause pain while urinating or during sex, as well as pain in the lower abdomen or testicles. Other symptoms include a foul-smelling genital discharge and abnormal vaginal bleeding. Chlamydia can cause significant damage to women’s reproductive systems and lead to serious pregnancy complications.
- Syphilis is another bacterial infection that affects more than the genitals. Throughout the stages of this infection, you can experience a rash, fever, fatigue, enlarged lymph nodes, body aches, and excessive soreness. If left untreated, syphilis can cause serious health problems over time.
- Hepatitis is an inflammatory condition of the liver, often caused by three viruses named for the disease: hepatitis A, B, and C. Symptoms include jaundice, dark urine, abdominal pain, fatigue, and other flu-like symptoms, and chronic infection can lead to cirrhosis, liver failure, and liver cancer.
- Human papillomavirus (HPV) is a common group of viruses that usually don’t cause any symptoms at all. However, some types of HPV can lead to the development of genital warts and, eventually, various types of cancer.
Each of these diseases becomes far worse if left untreated, leading to serious conditions like dementia, paralysis, blindness, infertility, birth defects, and liver failure. So, it’s important to get tested if you suspect you have one of these conditions.
However, the appearance of a sore on your genitals doesn’t automatically mean you’re living with genital herpes or another STI. For instance, certain relatively innocuous conditions can mimic the appearance of a herpes sore, such as:
- Ingrown hair: When a body hair grows down into the skin, it can cause an itchy or painful blister you might mistake for a genital herpes blister.
- Pimple: While not common, you can develop pimples in your genital region. However, herpes sores contain clear fluid rather the white pus found in pimples. The first outbreak of genital herpes also usually includes other symptoms, which are absent with pimples.
- Insect bite or sting: A bite from an insect may redden, swell, and itch. Excessive scratching can break the bite open, leaving behind a painful sore.
- Spider bite: A spider bite often looks a lot like an insect bite and is usually harmless. However, some spider bites can cause more serious symptoms, including severe pain and swelling or even an open sore.
- Jock itch: Excessive itchiness in the genital area can cause alarm, but jock itch is a fairly common condition that’s easily treatable with an antifungal medication.
2. Get Tested
Before worrying about the possibility of living with genital herpes, get tested to confirm the herpes simplex virus is the cause of your symptoms. A blood test is the most accurate and least expensive means of diagnosis.
Keep in mind that the herpes virus doesn’t always trigger outbreaks or other noticeable symptoms, so testing is an important way to monitor your health. The Centers for Disease Control and Prevention (CDC) recommends testing if you’re experiencing symptoms that could be related to herpes, or if you recently had sex with a new partner who has genital herpes.
A few different kinds of tests can determine whether you’re living with herpes:
- Tissue or herpes sore sample
- Polymerase chain reaction (PCR) to test for the presence of herpes DNA
- Tzanck smear test to find any active herpes virus on your genitals
- Blood test to detect the presence of antibodies to the herpes virus
Herpes tests can detect the virus even if you don’t have symptoms, so you don’t need to wait for an outbreak to get tested! However, talk with your healthcare provider about the best time to get tested; if it’s too soon after your exposure to the virus, the blood test may not detect the infection.
3. Educate Yourself About Herpes Myths
Myths about living with genital herpes are rampant, so it’s important to educate yourself about the herpes simplex virus and separate fact from fiction.
Myth: You Always Get a Herpes Outbreak Soon After Becoming Infected
Herpes is a sneaky infection. You can live with genital herpes in your body for months or even years without ever showing symptoms!
If you do develop an outbreak, it will most likely happen two to 12 days after your initial exposure to the virus. After they appear, blisters can take up to four weeks to fully heal.
Fortunately, subsequent outbreaks tend to be less intense. Recurring outbreaks are common, but they don’t last nearly as long at the first instance. Sores tend to heal within three to seven days, and the number of outbreak periods may even decrease over time.
Myth: If You Have a Cold Sore, You Have Genital Herpes
Cold sores and genital herpes are two distinct types of herpes infection. Many people get cold sores, but that doesn’t mean they have an STI or are living with genital herpes.
Herpes simplex virus type 2 (HSV-2) is the form of herpes virus categorized as a sexually transmitted infection (STI), and is the most common cause of genital herpes. It doesn’t usually cause cold sores, which are more often caused by HSV-1.
Cold sores from an HSV-1 infection don’t spread within your body to cause genital herpes. However, HSV-1 can cause genital herpes if it comes into contact with genital tissues. This can happen when a person touches their cold sore and then touches their own or someone else’s genitals, or during oral sex.
Researchers have seen an increase in the number of genital herpes cases caused by HSV-1 in recent years.
Myth: Your Partner Can’t Contract Genital Herpes Unless You Have an Active Breakout
The herpes virus is still contagious if you don’t have any sores on your body, or any symptoms at all. Even with no symptoms, if you’re living with herpes, the virus can still replicate and shed from your skin. This is called asymptomatic shedding.
You may experience more asymptomatic shedding if you’ve recently contracted genital herpes or if you have a compromised immune system. But no matter your individual circumstance, it’s always possible to spread the virus to a sexual partner. That’s why it’s important to always use safe sex practices even when no sores are present.
Myth: A Condom Provides 100% Protection Against Genital Herpes
Again, the herpes virus is always active in your body, even when no sores are present.
Wearing a condom is an important preventative measure if you or your sexual partner are living with genital herpes, but it doesn’t guarantee complete protection. The herpes virus lives in the skin both inside and outside the area a condom covers, so it can still spread from one person to another.
If you’re concerned about contracting or transmitting herpes, never have sex while you or your sexual partner have an active outbreak. The virus is more likely to spread when active sores exist. It’s also important that the infected person regularly take antiviral medicine to keep their infection under control.
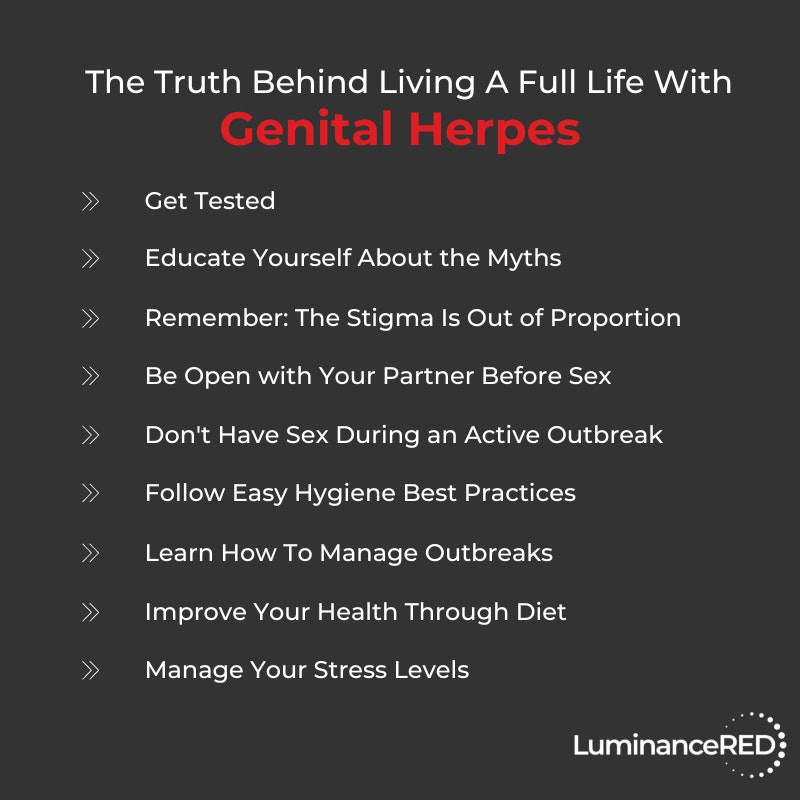
4. Remember: The Stigma Is Out of Proportion
The stigma around living with genital herpes is far more intense than the infection deserves. Genital herpes has been around for millennia, and HSV-2 is the most common STI in the United States. In fact, according to the World Health Organization, well over 400 million people worldwide are living with genital herpes.
The genital herpes stigma prevails largely because people don’t understand this condition. Many think they can catch genital herpes from a toilet seat or other common surfaces. They aren’t educated about how HSV-2 spreads or affects the body. Others don’t know that genital herpes remains dormant for months and years at a time, allowing those living with herpes to lead completely normal lives.
Overall, genital herpes can be a highly manageable condition, with few physical side effects. In fact, your outbreaks may be so infrequent or mild that you barely notice the virus at all. Some people don’t experience symptoms until years after their first outbreak!
5. Be Open With Your Sexual Partner
If you have a confirmed or suspected HSV-2 infection, it’s important to make sure your sexual partner is informed before being sexually intimate.
Condoms can help keep the virus from spreading, but they don’t prevent all transmission during sex. In fact, the transmission of HSV-2 via oral sex is possible even if there are no sores present on the genitals or mouth.
Though it’s impossible to completely eliminate the chance of transmission short of abstaining from sexual contact, prevention techniques are very effective. For example, one large study reported that only 1.9% of susceptible sexual partners became infected with clinically symptomatic HSV-2 when given the antiviral valacyclovir as a precautionary treatment.
It’s essential to be open and honest with your sexual partner. By improving communication, educating yourselves, and managing expectations, you can better reduce the risk of spreading a genital herpes infection.
6. Don’t Have Sex During an Active Outbreak
When living with genital herpes, you can greatly limit the risk of transmission by refraining from intimate contact until a herpes outbreak clears and heals completely. The virus is highly contagious for your sexual partner from the time your first sores develop until your outbreak has completely scabbed and healed.
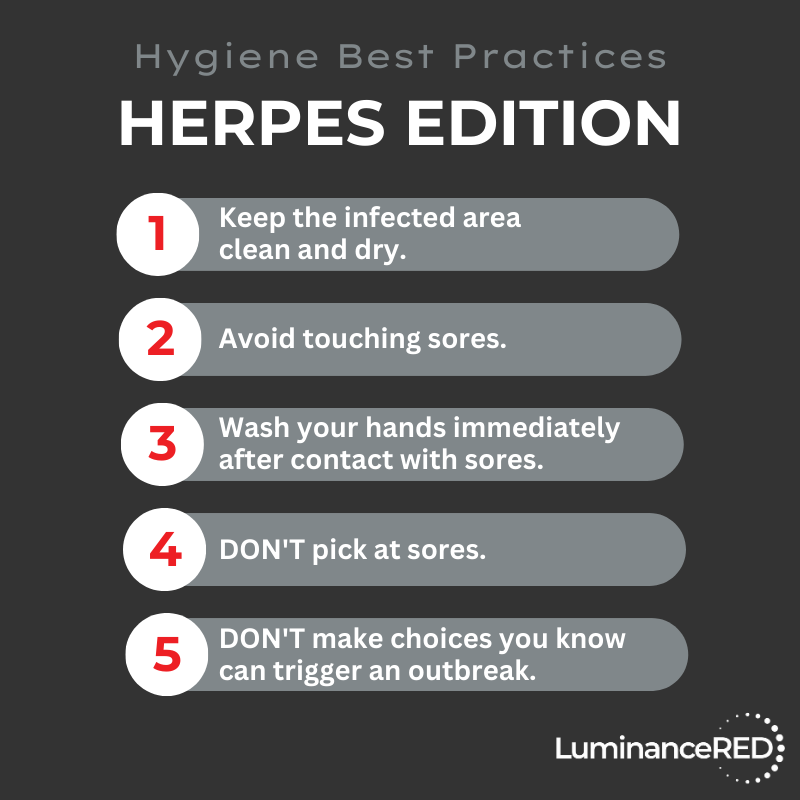
7. Follow Easy Hygiene Best Practices
Following these simple hygiene best practices is an easy preventative measure to avoid accidentally spreading the virus to a sexual partner:
- Keep the infected area clean and dry.
- Avoid touching sores.
- Wash your hands immediately after any possible contact with sores.
- DON’T pick at the sores. This can cause infection and contaminates your hands.
- DON’T make choices you know can trigger an outbreak.
8. Learn How to Manage Outbreaks
While there’s no cure for genital herpes, a lot can be done to reduce the length and severity of outbreaks.
A number of proven medications speed up the healing process and reduce discomfort. Prescription antiviral medications like acyclovir and valacyclovir help control and minimize herpes outbreaks.
Start taking acyclovir as soon as you notice the first signs of an emerging outbreak. This medication stops the herpes virus from growing and spreading through your cells, though it can’t remove the virus from your body completely. Most people living with herpes experience relief within just a few days.
Improving lifestyle habits may also prevent future herpes outbreaks:
- Get lots of rest to support a strong immune system.
- Eat nutritious foods to support your body’s innate healing response.
- Manage stress.
9. Improve Your Health Through Diet
Foods that contain high levels of vitamin C and other inflammation-fighting nutrients can alleviate the symptoms of HSV-2.
Clinical and anecdotal research show these foods and supplements in particular may help prevent herpes outbreaks:
- Lean protein
- Omega-3 fatty acids
- Zinc
- Lysine
- Probiotics
- Vitamin B complex
At the same time, avoid foods thought to encourage outbreaks, such as excessive alcohol, sugar, and refined carbohydrates.
10. Manage Your Stress Levels
Existing research suggests a high correlation between genital herpes outbreaks and persistent anxiety, depression, and psychological stress.
Beyond the standard advice to eat better, sleep more, and avoid alcohol, these techniques can help you cope with ongoing stress and anxiety:
- Mindfulness
- Deep breathing exercises
- Grounding techniques
- A change in surroundings
- Helping others
- Delegating small tasks to others
- Talking to a professional
Living With Genital Herpes
Now that you know the top 10 ways to make living with herpes easier, let’s go through the best treatment options to help ensure you have the highest possible quality of life.
Obviously, your first step is a proper diagnosis from your healthcare professional. During this appointment, you will likely learn some of the options for prescription medications to treat genital herpes. The popular valacyclovir can treat active outbreaks and help reduce the chance of spreading genital herpes to your sexual partners. Your doctor can help you decide which medication is best for you if you’re living with genital herpes.
There are also a variety of over-the-counter medications that can help. These include topical treatments to help ease symptoms during active breakouts and pain relievers to make living with herpes a little easier.
If you prefer to go the natural route, there are a number of home remedies you can try, including:
- Coconut oil
- Epsom salt bath
- Baking soda
- Corn starch
- Apple cider vinegar
- Rubbing alcohol
- Garlic
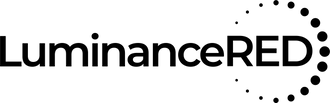
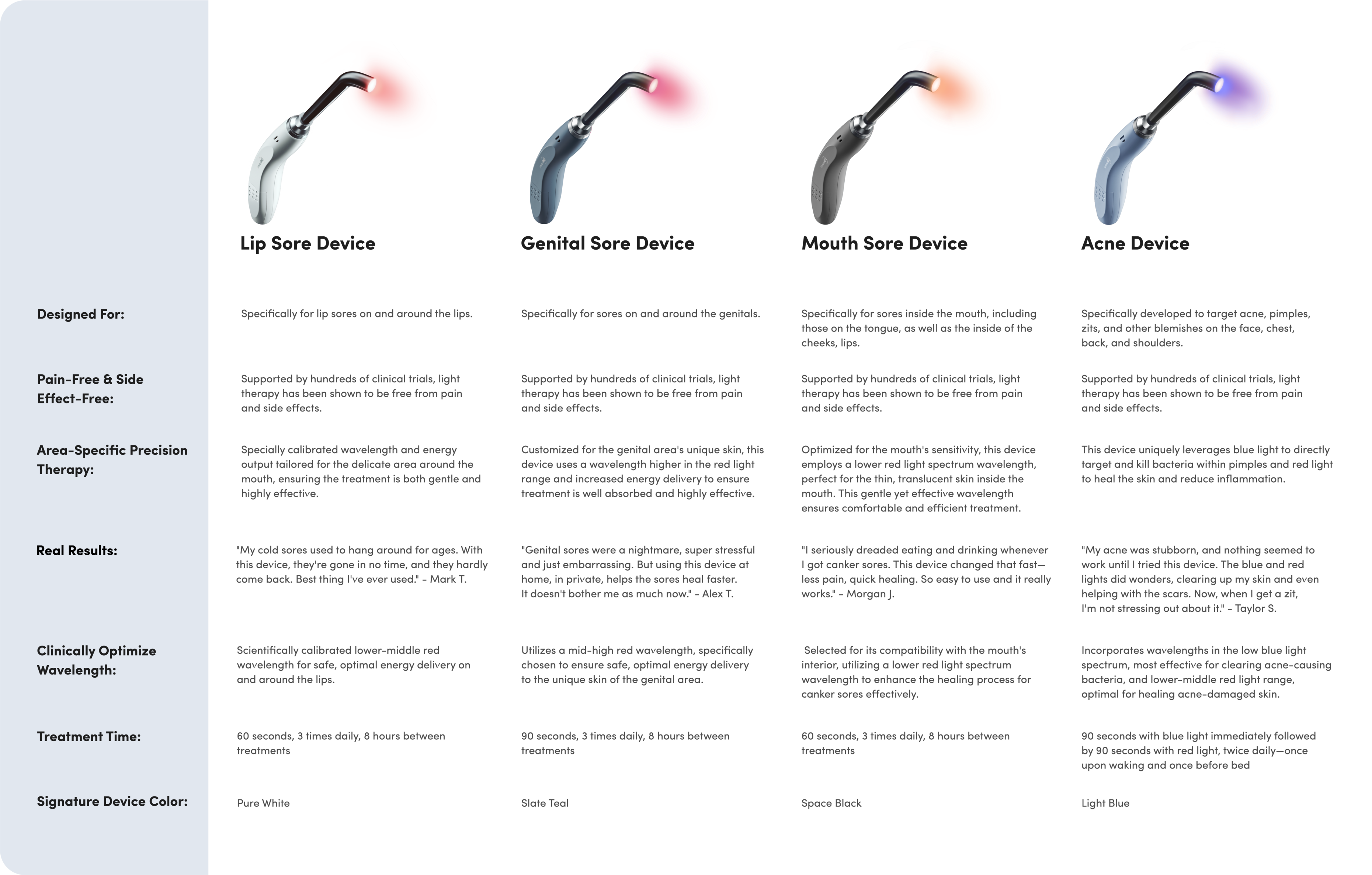
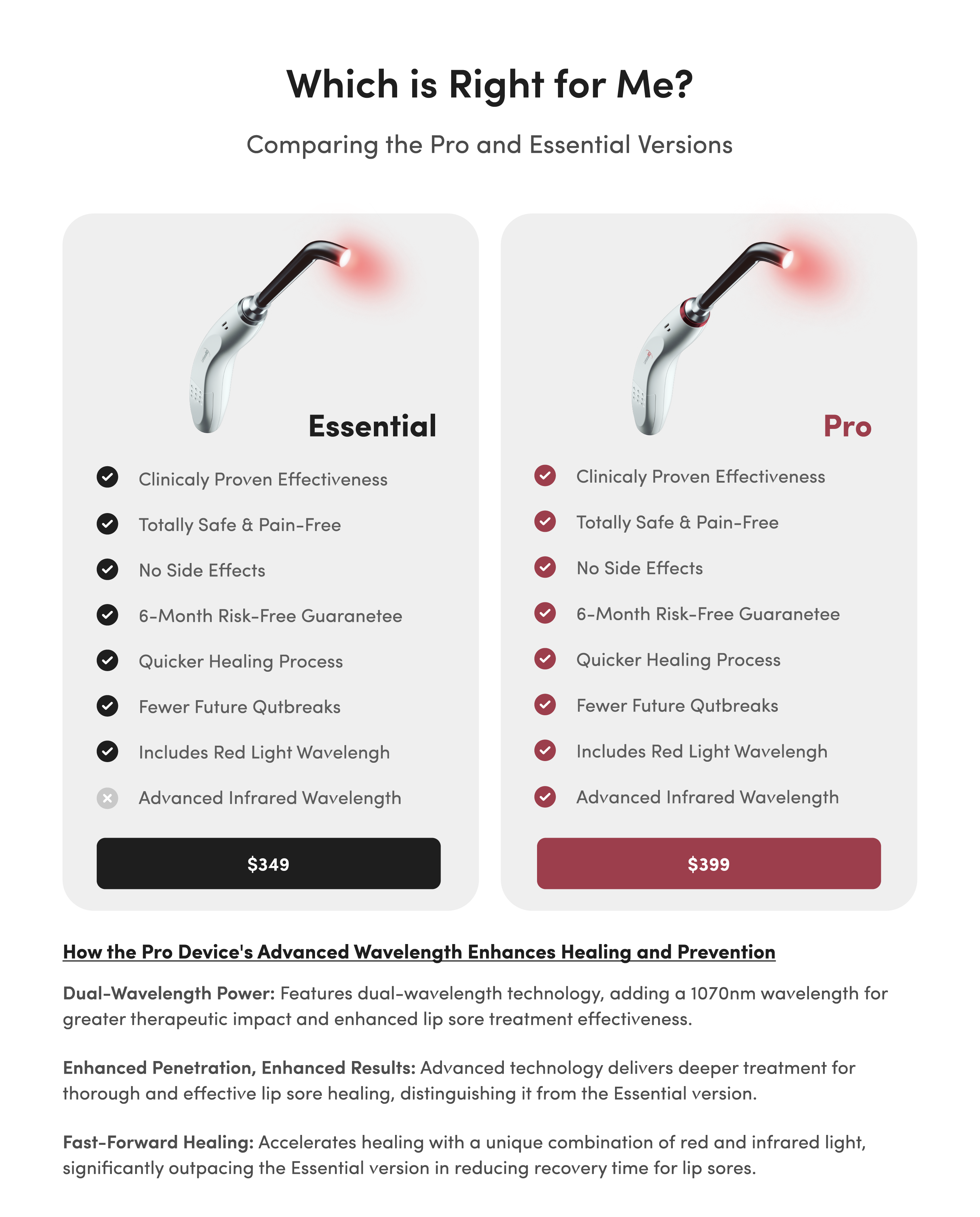
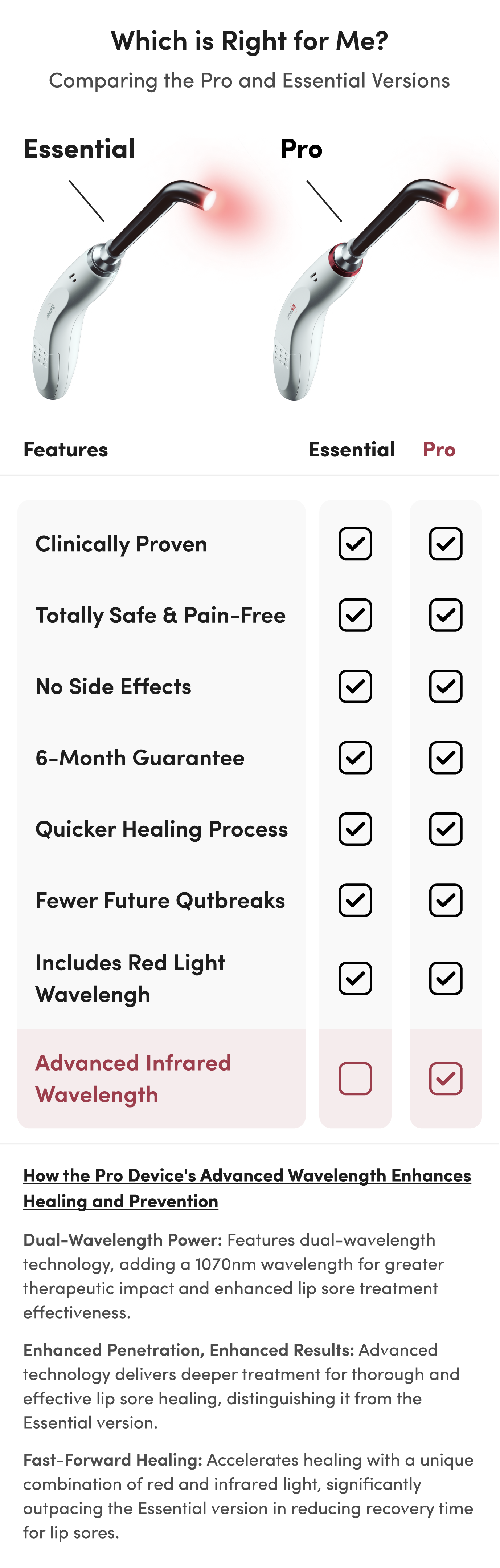
If you’d like a natural remedy that doesn’t involve applying anything directly to the sores, consider light therapy. Clinical studies indicate that light therapy can help reduce the pain, severity, frequency, and viral load of genital herpes outbreaks.
Home devices, like the Luminance RED Genital Sore Treatment Device, are available, allowing you to treat your outbreak in privacy and giving you more control over living with herpes. They nourish the skin with medically optimized red light, which accelerates cellular healing processed and strengthens defenses against future attacks. Regular use of red light therapy not only shortens the healing time of active outbreaks, but can dramatically extend the time between future outbreaks!
Though there isn’t a cure for genital herpes, these 10 tips can help you live your life to its fullest. There’s no reason HSV-2 should keep you from living a satisfying and fulfilling life!