HSV-1 vs. HSV-2: Separating Facts from Myths
Myths about how people contract herpes creates unnecessary confusion around this common viral infection. The basics: genital herpes (HSV-2) is most often transmitted through intimate contact with a sexual partner, and cold sores (HSV-1) can quickly be spread via simple touch. Both types of herpes share common symptoms and characteristics, but each one has unique triggers and modes of transmission.
What Triggers HSV-1 vs. HSV-2?
Herpes is a lifelong illness. The virus lies dormant in the body's sensory nerve ganglia located in the temples (HSV-1) or the base of the spine (HSV-2). When something irritates the nerves, the virus reactivates, travels through the nerve pathways, and causes an outbreak or viral shedding without symptoms. Herpes outbreaks tend to last 7-10 days, but lesions may take 2 weeks to fully heal.
Many people with HSV-1 find that cold sores develop in the same areas. Common triggers include:
- Exposure to harsh sunlight
- Biting or chewing on the lips
- Irritating toothpaste or mouthwash
- Parasitic infestations of the gut
- Injury to the lips from activities like sports
HSV-2 is a sexually transmitted disease (STD). Like HSV-1, HSV-2 lesions tend to appear in the same places, but outbreaks don't occur as often. HSV-2 outbreaks are often linked to:
- Frequent sex and intimate activities involving friction
- Irritating personal care products (pads, laundry detergent)
- Contracting common STIs such as gonorrhea
- Wearing tight pants and underwear
Both types of herpes share common triggers. HSV-1 and HSV-2 are both inflamed by stressful life events, poor diet (particularly foods rich in L-arginine), lack of sleep, hormonal fluctuations, underlying autoimmune conditions (HIV/AIDS, Bechet's, SLE, Crohn's), and menstruation.
Are Cold Sores an STD?
If you see a strange bump on your lip you might wonder, is it an HSV-1 cold sore or HSV-2 lesion? Know this: cold sores are herpes, but having herpes doesn't mean you have an STD.
HSV-1 is transmissible through oral sex, but it affects people of all ages regardless of sexual activity. Infants and children often develop cold sores through close contact (kissing, skin-to-skin) with an adult who has the Herpes Simplex Virus, so HSV-1 isn't technically an STD. The vast majority of people with HSV-1 contract the virus before they become sexually active.
Pregnant women can pass the virus onto their unborn children, though the risk of transmission is highest for women who contract the virus during pregnancy. Women who have had the virus for long periods of time are less likely to pass it on.
Common Causes of HSV-1 vs. HSV-2
HSV-1 and HSV-2 can be contracted in similar ways. Both types of herpes are transmitted through close contact, especially with an individual experiencing an outbreak. These activities put you at high risk of contracting HSV-1 if you're exposed to someone who has the virus:
- Kissing them on the mouth or cheek
- Touching a lesion and then touching your lips
- Immediately using the same cup or straw
- Swapping lip balm, lipstick, and facial razors
It's uncommon but not impossible to contract HSV-2 through oral sex. This type of herpes is most often transmitted through genital-to-genital contact, anal sex, and vaginal sex. In exceptionally rare cases, HSV-2 can be transmitted by sharing bath towels and underwear with someone who tested positive.
4 Herpes Simplex Myths, Debunked
The Internet is filled with misinformation about the differences between HSV-1 vs. HSV-2 and how to manage these lifelong conditions. If you or your loved one was recently diagnosed with herpes, or you want to protect yourself, understand these common herpes myths.
You can only have one type of herpes
It's possible to have both strains of herpes. HSV-1 typically occurs on and around the lips, while HSV-2 most often affects the genitals, buttocks, groin, and inner thighs. However, up to 40% of genital herpes outbreaks are caused by HSV-1 and concurrent infections are common. In other words, having HSV-1 doesn't decrease your chances of contracting HSV-2.
Herpes always causes a quick initial outbreak
Not everyone who contracts herpes experiences the infamous initial outbreak right away. In fact, herpes can lie dormant for years before symptoms appear - if they appear at all.
The initial outbreak is most likely to occur in the herpes incubation window, which typically lasts 2-12 days after exposure. Many people report experiencing flu-like symptoms during their first outbreak, such as swollen lymph nodes, fatigue, and GI issues. Lesions can be extremely painful and take around 2-4 weeks to heal. Future outbreaks tend to be less severe.
Using condoms prevents herpes
Research has shown that condoms only decrease your chances of contracting herpes by 30% if used correctly 100% of the time. With a relatively high failure rate, condoms can expose you or your partner to herpes by slipping off, breaking, or exposing part of the penis during sex. Furthermore, condoms don't protect you or your partner from herpes lesions on the testicles and groin.
Herpes outbreaks look like blisters
Painful clusters of pus-filled blisters on the lips or genitals are classic signs of herpes. But some people develop a stronger immunity to the virus, which leads to mild outbreaks that don't resemble sores. HSV-1 might look like an ingrown facial hair, a cut on the lip, or a small pimple. Similarly, HSV-2 outbreaks are commonly mistaken for ingrown hairs and irritated skin.
Differences Between Treating HSV-1 vs. HSV-2
From honey to aloe vera, there are countless home remedies for herpes. Most people find that medication works better for preventing debilitating herpes outbreaks.
HSV-1 is typically managed with over-the-counter topical treatments. Their numbing agents relieve itchiness and burning, but they don't stop outbreaks. Valtrex and Acyclovir are popular oral medications for HSV-2, but they only shorten the length of herpes outbreaks by a few days. They also come with side effects such as drowsiness, nausea, vomiting, hair loss, and headaches.
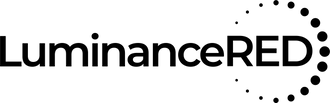
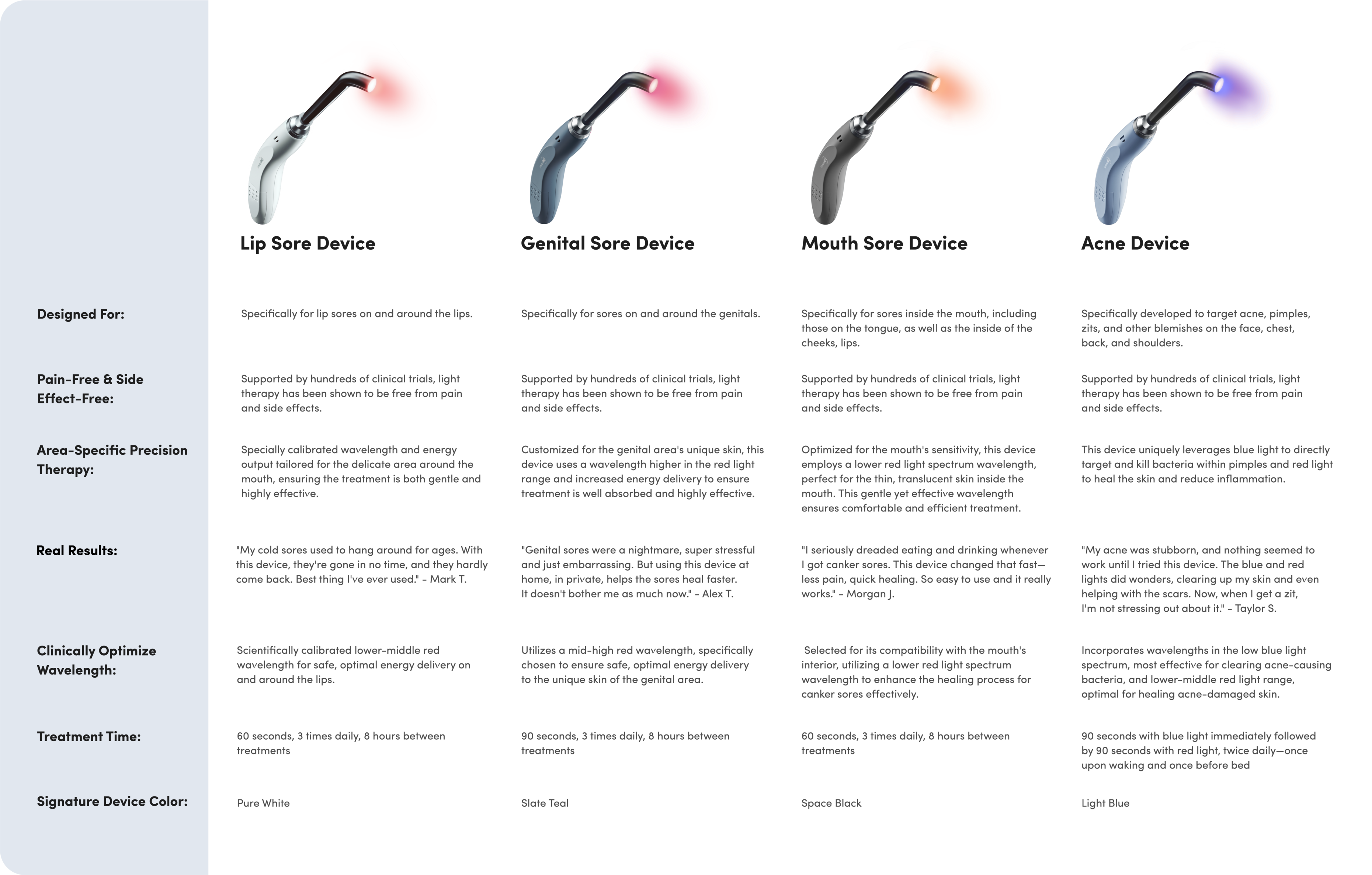
Healing herpes with red light therapy
Your treatment options for herpes aren't limited to hit-or-miss topicals and ineffective home remedies. The Luminance RED is an FDA registered device that uses gentle red light therapy to treat and prevent future cold sore and genital herpes outbreaks. Hold the Luminance RED on areas where you tend to develop lesions for 60 seconds, twice per day. The red light soothes nerve pathways where outbreaks take root. With the Luminance RED, going into hiding for days and caking concealer over cold sores will become troubles of the past.